Integrated Care: What Choices Exist for Californians with Medicare and Medi-Cal?
summary
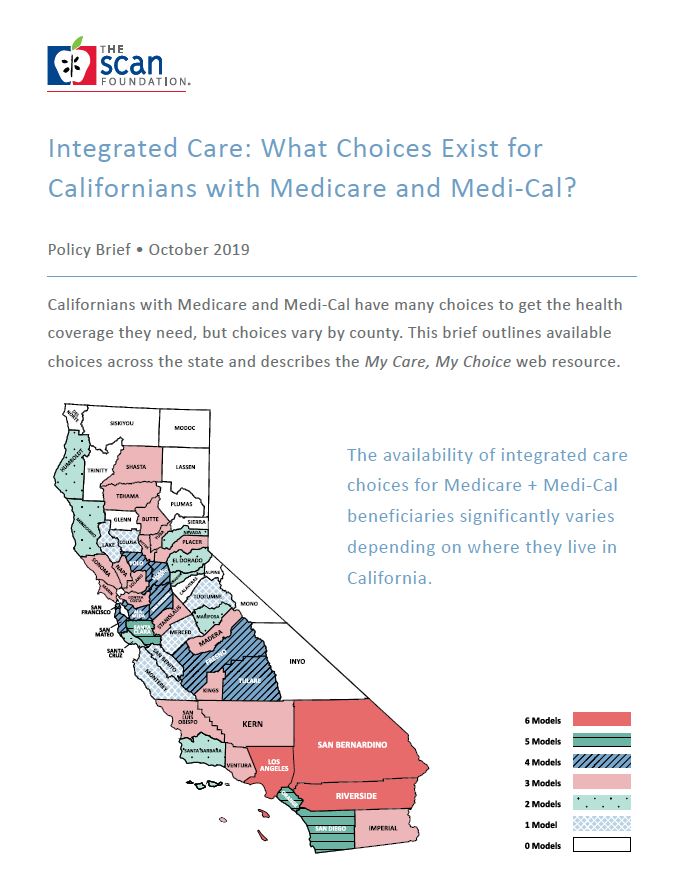
Californians with Medicare and Medi-Cal have many choices to get the health coverage they need, but choices vary by county. This brief outlines available choices across the state and describes the My Care, My Choice web resource.
Date Updated: 10/16/2019Introduction
Californians with Medicare and Medi-Cal (also known as dually eligible individuals) have many choices to get the health care and long-term services and supports (LTSS) they need. This is a unique and diverse group of individuals with low incomes and high needs who account for a disproportionately large share of spending in both Medicare and Medi-Cal. Recent innovations in Medicare, along with shifts in Medi-Cal to a managed care delivery system, have created more choices in how care is delivered for people who qualify for both programs. However, choices of how Medicare and Medi-Cal work together vary by county, so it can be confusing for individuals to decide which care option best meets their unique needs. Californians with Medicare and Medi-Cal deserve to know their local coverage choices because decisions on how to use their health coverage can affect the access to providers. For example, individuals can have a doctor or network of providers who coordinate his/her medical and non-medical health related services and supports—often called integrated care. Individuals can use their Medicare to choose a doctor in a private practice, medical group, or health plan. However, individuals often do not know about available options or how to access integrated care. This brief outlines the range of integrated care choices available to the 1.4 million Californians with Medicare and Medi-Cal.1 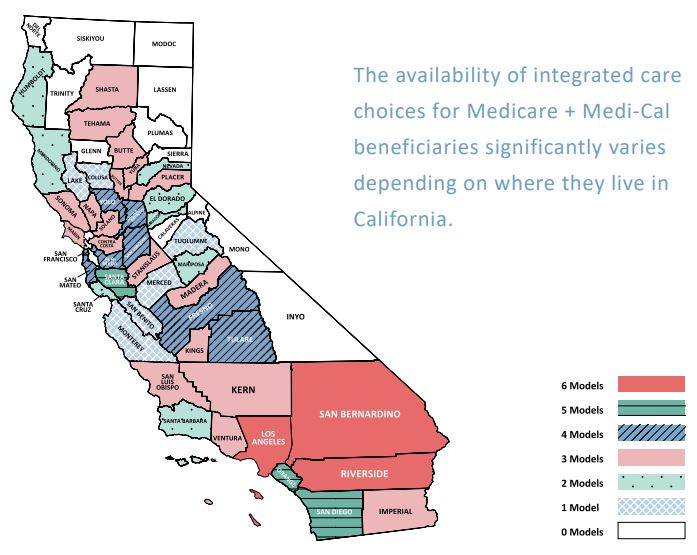
Medicare and Medi-Cal basics
Medicare is a federal health insurance program for people age 65 and older and those younger than 65 with a disability. Medicare provides coverage for hospital care (Part A), medical services (Part B), and prescription drugs (Part D). An individual can access benefits through the original fee-for-service Medicare, which is available nationwide. In original Medicare, individuals can visit any provider who accepts Medicare, and payments are made directly to providers on a fee-for-service basis. With original Medicare, individuals must find their own doctors, hospitals, and other care providers, sign up for a separate plan for prescription drugs, and there are no extra benefits like care coordination. The other choice is a Medicare managed care plan, where available by geographic area. Here, individuals choose providers who are contracted with the plan, and referrals are generally needed to visit a specialist in the plan’s network. Individuals in a managed care plan generally receive additional benefits beyond original Medicare. The plans are paid a fixed monthly rate to manage an individual’s total health care needs. There are several types of Medicare managed care plans for individuals with complex care needs, which are described later in this brief.2,3 For services that both Medicare and Medi-Cal can cover (e.g., doctors’ visits, hospital care, skilled nursing care), Medicare pays first and Medi-Cal pays second to cover any remaining costs, including Medicare co-insurances and copayments.3,5
What is integrated care?
When people have two forms of health coverage such as Medicare and Medi-Cal, there can be inefficiencies in how care is paid for and provided. Recent federal health care efforts focused on integrating Medicare and Medicaid to make care from these programs more efficient and seamless. 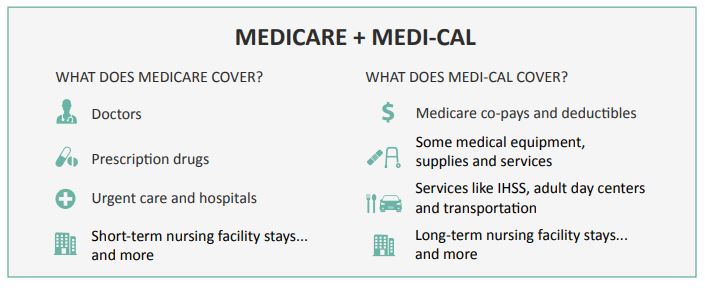 Integrated care means that an individual can access medical care and non-medical services by working through one lead entity that is responsible to provide and/or organize care. In integrated care, the health care entity uses care coordination to connect the individual to a range of services and supports to meet his/her overall needs. The degree to which Medicare and MediCal services are integrated depends on the range of services provided and coordinated, contractual arrangement across various providers, and degree of blended funding. The least comprehensive choices focus solely on coordinating medical care (e.g., primary and specialty care). The most comprehensive choices help connect individuals with services and supports in their local communities (e.g., meals, home modifications, county-based behavioral health services), and may provide additional benefits beyond the core coverage of Medicare and Medi-Cal. For this paper, we define the degrees of integration as follows. Modest: Core medical services are provided and coordinated through a network of health providers that has a structured agreement to communicate and share information for purposes of coordinating services. Medicare and Medi-Cal funding streams are separate. Moderate: A health system is responsible for providing services funded through the primary coverage (most often Medicare), while coordinating the range of medical services, behavioral health services, and LTSS covered by both Medicare and Medi-Cal. Services are typically provided through a network of providers contracted with the health plan. Medicare and MediCal funding streams are separate. Most: One health system is responsible for providing and coordinating all covered medical services, behavioral health services, and LTSS covered by both Medicare and Medi-Cal. Services are typically provided through a network of providers contracted with the health plan. Medicare and Medi-Cal funding is blended—managed by a single plan.
Integrated care means that an individual can access medical care and non-medical services by working through one lead entity that is responsible to provide and/or organize care. In integrated care, the health care entity uses care coordination to connect the individual to a range of services and supports to meet his/her overall needs. The degree to which Medicare and MediCal services are integrated depends on the range of services provided and coordinated, contractual arrangement across various providers, and degree of blended funding. The least comprehensive choices focus solely on coordinating medical care (e.g., primary and specialty care). The most comprehensive choices help connect individuals with services and supports in their local communities (e.g., meals, home modifications, county-based behavioral health services), and may provide additional benefits beyond the core coverage of Medicare and Medi-Cal. For this paper, we define the degrees of integration as follows. Modest: Core medical services are provided and coordinated through a network of health providers that has a structured agreement to communicate and share information for purposes of coordinating services. Medicare and Medi-Cal funding streams are separate. Moderate: A health system is responsible for providing services funded through the primary coverage (most often Medicare), while coordinating the range of medical services, behavioral health services, and LTSS covered by both Medicare and Medi-Cal. Services are typically provided through a network of providers contracted with the health plan. Medicare and MediCal funding streams are separate. Most: One health system is responsible for providing and coordinating all covered medical services, behavioral health services, and LTSS covered by both Medicare and Medi-Cal. Services are typically provided through a network of providers contracted with the health plan. Medicare and Medi-Cal funding is blended—managed by a single plan.
What are the choices in California?
California has six different care choices to help individuals make the most of their Medicare and Medi-Cal coverage. Brief descriptions are provided below, and are ordered by degree of integration from modest to most integrated
Accountable Care Organization (ACO)
Medicare ACOs are groups of doctors, hospitals, and other providers that work together to provide care for people with original Medicare. If an ACO provides quality care and achieves savings for the Medicare program, the ACO is rewarded with a portion of the savings. To facilitate coordination, Medicare shares certain health information with the ACO (e.g., medical conditions, prescriptions, doctor visits). However, individuals do have a choice as to whether their health information is shared within the ACO network. To participate in ACO services, individuals select a primary clinician that is part of an ACO, or are assigned to an ACO based on utilization of medical services. The benefit to the individual is seamless coordination of Medicare services with all providers having access to the same medical information, creating fewer burdens for the individual and caregiver. In California, there is no requirement for ACOs to coordinate with Medi-Cal services. Individuals involved in an ACO continue to have the same rights of original Medicare, including the right to choose any doctors and providers that accept Medicare.6-8 ACOs are available in 36 counties.9
Medicare Advantage (MA)
An MA plan, also known as Medicare Part C, is a private health insurance company paid by Medicare to provide all covered Medicare benefits (Parts A and B) for individuals who enroll in the plans. Most MA plans also offer prescription drug coverage (Part D). Some MA plans, such as health maintenance organizations (HMOs) and preferred provider organizations (PPOs), are referred to as “coordinated care plans” and seek to coordinate an individual’s health care needs within the health plans’ network of providers. For the purposes of this paper, references to MA are specifically focused on the HMO and PPO coordinated care plans.2 People who have both Medicare and MediCal can have an MA plan for their Medicare and a Medi-Cal managed care plan for their MediCal. This means they will be working with two different health plans, and the MA plan will only coordinate Medicare services. MA plans are available in 42 counties.10
Dual Eligible Special Needs Plan (D-SNP)
A D-SNP is a type of MA plan for individuals with Medicare and Medi-Cal. The health plan is responsible for providing all Medicare benefits (including prescription drug coverage), and providing or arranging for Medi-Cal-covered services to the extent required by the state. In California, D-SNPs do not provide LTSS, but they are responsible for ensuring that individuals receive all services covered under both Medicare and Medi-Cal. To do this, the plan assesses an individual’s needs and develops a care plan. A D-SNP may also offer extra benefits beyond what Medicare traditionally covers.11 With this option, individuals would have just one health plan for both Medicare and MediCal, though it would not cover LTSS. D-SNPs are available in 36 counties.10
Fully Integrated Dual Eligible Special Needs Plan (FIDE SNP)
A FIDE SNP is a type of MA plan for individuals with Medicare and Medi-Cal that includes all covered benefits, as well as some extra benefits. To qualify, individuals must be certified to need nursing home care, but are living in the community. This health plan is different than a D-SNP because it integrates and coordinates all Medicare and Medi-Cal benefits, including LTSS, under one health plan.11 A care coordinator is provided to help high-risk individuals navigate the delivery system. A FIDE SNP is available in three counties.10
Cal MediConnect (CMC)
Cal MediConnect is a type of health plan that includes all Medicare and Medi-Cal benefits, including LTSS. Individuals enrolled in a CMC health plan have the opportunity for services to be coordinated, meet with an interdisciplinary care team, and receive optional benefits offered beyond what Medicare and Medi-Cal traditionally offer. Californians with Medicare and Medi-Cal who do not choose a CMC plan must select a Medi-Cal Managed Care plan for their LTSS benefits, an arrangement known as managed LTSS (MLTSS).* CMC plans and MLTSS are available in seven counties.12
Program of All-Inclusive Care for the Elderly (PACE)
PACE is a health plan, funded by both Medicare and Medi-Cal, to provide and coordinate all covered medical and LTSS. PACE serves individuals who are age 55 and older and certified to need nursing home care, but who are able to live safely in the community at the time of enrollment. A core component of this model is the use of an interdisciplinary team that assesses participants’ needs, develops care plans, and delivers all services. PACE provides services primarily in a CommunityBased Adult Services (CBAS) center (also known as an adult day health center), supplemented with other community-based services to meet the individual’s needs. Individuals enrolled in PACE must see providers in the PACE network.14-15 PACE is available in 17 counties.10 The figure below shows the continuum of California’s six integrated care models from a modest degree to the most integrated. 
What are the differences between California’s integrated care choices?
Californians with Medicare and Medi-Cal have many choices for their health care coverage. Participation in the different coverage choices varies by age and level of functional need. The range of coverage choices varies in the benefits offered, and is influenced by type of coverage (particularly whether Medi-Cal services are or are not included in the model), program structure, and needs of the population served. All choices allow an individual to use their Medicare and Medi-Cal benefits. Some choices provide services through a network of providers, whereas others provide services through an onsite location (e.g., PACE). Some individuals like choices that put Medicare and MediCal benefits together into one health plan, while others like using original Medicare. Understanding the main differences can help individuals select the model that best meets their needs. Table 1 compares the main differences between the coverage choices.ᵻ
Where are integrated care models located in California?
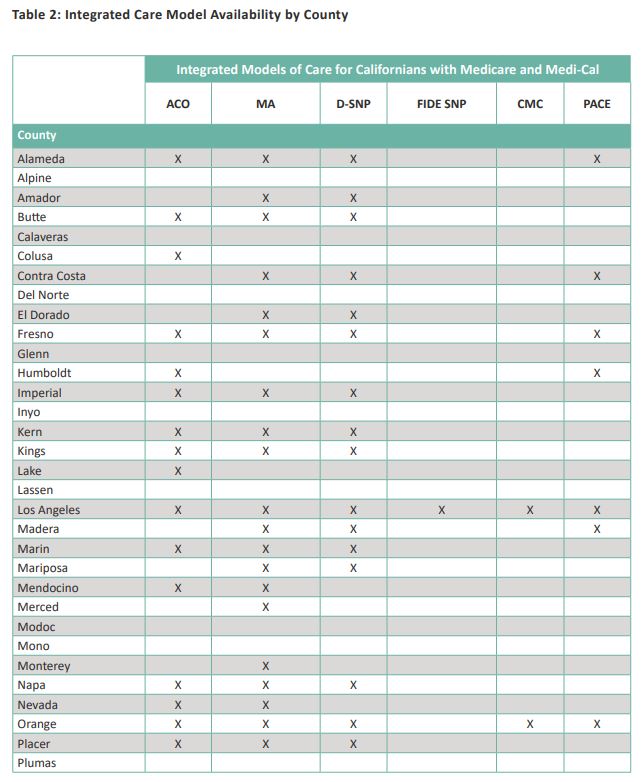
Where an individual lives matters when accessing integrated care choices. While Medicare and Medi-Cal are available in all counties, only 46 counties have at least one integrated care choice. This can create challenges for Californians in understanding the available choices (particularly those in rural areas), as well as how they can participate in the best model for them. Table 2 shows where integrated care models are offered in California’s 58 counties as of October 2019.10 

How can Californians find out about their local care choices?
While Californians with Medicare and Medi-Cal have many options to get their health care, figuring out which options might be a “best fit” can be really confusing. My Care, My Choice is a unique website designed to help Californians with Medicare and Medi-Cal explore health care coverage choices based on their location, their needs, and what they want from their coverage. Currently available in four languages, it allows individuals to learn about the range of care options in their area so they can get the most from their health care coverage. By answering a few questions, My Care, My Choice provides a list of local care choices to fit a person’s care needs and preferences. My Care, My Choice was developed by The SCAN Foundation and its partners using federal and state data. 
Conclusion
Californians with Medicare and Medi-Cal have many choices when it comes to their health care coverage, but the choices available vary depending on where an individual lives. Figuring out what options are available in a given area and understanding the key differences to make an informed choice can be challenging. Selecting the health care model that best meets a person’s needs may require consideration of factors beyond medical, such as services available and the level to which there is help to navigate those services. This brief presents information about California’s different integrated care choices, to help Californians with Medicare and Medi-Cal, trusted advisors, and policymakers learn about the range of care options in their local area so individuals can get the most from their health care coverage. This brief also identifies areas of the state where there are little or no integrated care choices, and shows opportunities for growth.
Download the publication for all visuals and complete references.
Continue Reading
This policy brief provides an introduction to The SCAN Foundation’s CLASS Technical Assistance Brief Series, which explores many of the critical issues to be considered for successfully implementing CLASS.
This policy brief describes the broad needs of individuals with disability and the wide range of supportive and environmental solutions that can allow for the most independent living possible. It suggests how findings on social and environmental supports for individuals with disability can inform implementation of CLASS.
This policy brief provides background on the historical development of benefit eligibility triggers in the private long-term care insurance market. Understanding how these triggers came into being can provide important information to those charged with implementing the CLASS Plan.