10 Things to Discuss With Your Doctor to Promote Aging with Dignity and Independence
summary
Having regular conversations with your doctor is an important component of aging with dignity and independence. This guide describes important conversations to have with your doctor to prepare for changing health needs as you grow older.
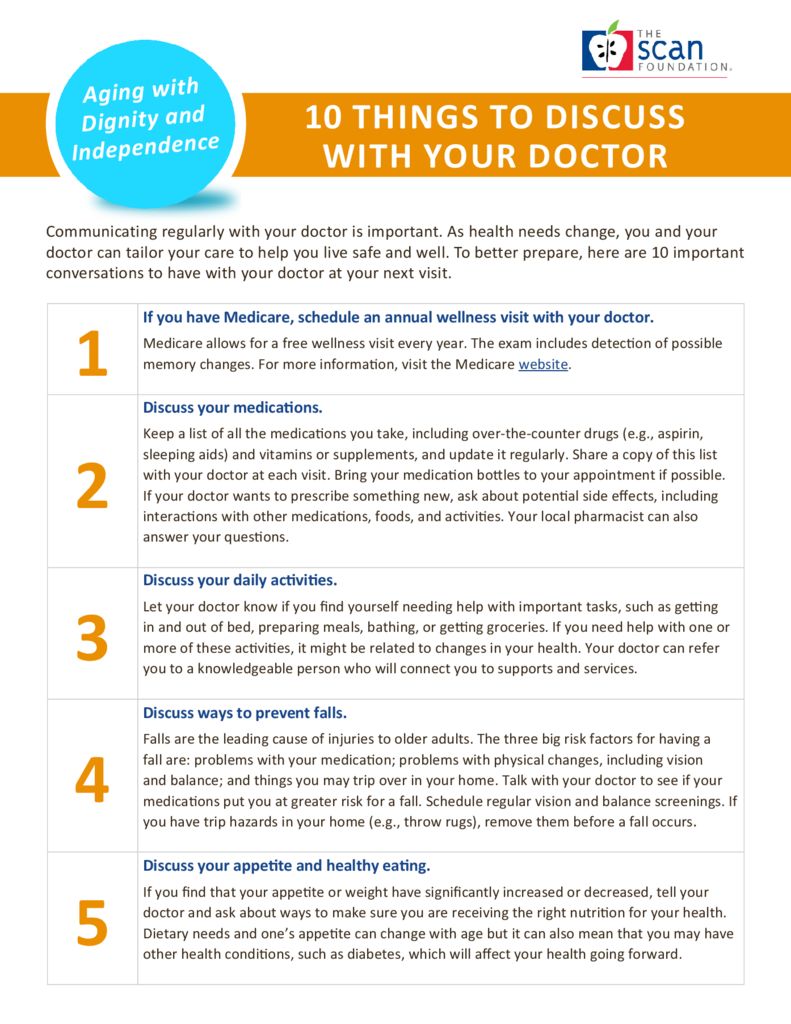
Date Updated: 03/01/2013Communicating regularly with your doctor is important. As health needs change, you and your doctor can tailor your care to help you live safe and well. To better prepare, here are 10 important conversations to have with your doctor at your next visit.
- If you have Medicare, schedule an annual wellness visit with your doctor.
Medicare allows for a free wellness visit every year. The exam includes detection of possible memory changes. For more information, visit the Medicare website. - Discuss your medications.
Keep a list of all the medications you take, including over-the-counter drugs (e.g., aspirin,sleeping aids) and vitamins or supplements, and update it regularly. Share a copy of this list with your doctor at each visit. Bring your medication bottles to your appointment if possible.If your doctor wants to prescribe something new, ask about potential side effects, including interactions with other medications, foods, and activities. Your local pharmacist can also answer your questions. - Discuss your daily activities.
Let your doctor know if you find yourself needing help with important tasks, such as getting in and out of bed, preparing meals, bathing, or getting groceries. If you need help with one or more of these activities, it might be related to changes in your health. Your doctor can refer you to a knowledgeable person who will connect you to supports and services. - Discuss ways to prevent falls.
Falls are the leading cause of injuries to older adults. The three big risk factors for having a fall are: problems with your medication; problems with physical changes, including vision and balance; and things you may trip over in your home. Talk with your doctor to see if your medications put you at greater risk for a fall. Schedule regular vision and balance screenings. If you have trip hazards in your home (e.g., throw rugs), remove them before a fall occurs. - Discuss your appetite and healthy eating.
If you find that your appetite or weight have significantly increased or decreased, tell your doctor and ask about ways to make sure you are receiving the right nutrition for your health.Dietary needs and one’s appetite can change with age but it can also mean that you may have other health conditions, such as diabetes, which will affect your health going forward. - Discuss your ability to concentrate and how you are feeling.
We all have “moments of forgetfulness”. But if forgetting things has become more common, tell your doctor as soon as possible. There may be an underlying health or medication related reason. Also, everyone experiences changes in moods, including sadness. Yet if you feel more anxious or upset than usual, find it hard to concentrate, or have trouble sleeping for more than two weeks, be sure to tell your doctor. - Discuss possible specialty care for ongoing health conditions.
If you have an ongoing health condition that is affecting your daily life (e.g., arthritis), talk with your doctor about a specialist or specialty services that may help. If you decide this is the right course, make sure that the specialist keeps your regular doctor informed of changes to your medications or treatment, and update the lists you keep. - If you’re in the hospital…
If you find yourself in the hospital unexpectedly, make sure that the hospital care team keeps your regular doctor informed about your care and plans for returning home. When planning to leave the hospital, ask the following questions:- Will I need any follow-up care? If so, what is it, with whom, and how often?
- Will my medication regimen change when I leave? If so, how?
- Are there any warning signs I should watch out for when returning home, and what should I do if these occur?
- Discuss your health care preferences and choices.
Let your doctor know about your care preferences to create the best plan for your health and well-being if you cannot make decisions on your own behalf. Strongly consider filling out documentation that designates another person to make health care decisions on your behalf if you become unable, and an advance directive (i.e., living will) describing your care wishes if you cannot communicate these decisions. Make sure your doctor and designee have copies of each. One tool is Five Wishes, which can help you clarify and communicate your wishes. - Discuss services in your community that may help.
Most communities have services to help people manage health conditions and get the support they need. Your doctor may know about classes or community programs that help people with specific health conditions, such as diabetes management or cancer support groups. Your doctor may also have staff knowledgeable about the range of services in your community, so keep your doctor aware of your needs as they change in order to live well.
Continue Reading
This policy brief provides an introduction to The SCAN Foundation’s CLASS Technical Assistance Brief Series, which explores many of the critical issues to be considered for successfully implementing CLASS.
This policy brief describes the broad needs of individuals with disability and the wide range of supportive and environmental solutions that can allow for the most independent living possible. It suggests how findings on social and environmental supports for individuals with disability can inform implementation of CLASS.
This policy brief provides background on the historical development of benefit eligibility triggers in the private long-term care insurance market. Understanding how these triggers came into being can provide important information to those charged with implementing the CLASS Plan.