Ensuring Quality: The Path to Creating Measures and Engaging Stakeholders
summary
This policy brief provides an overview of the various types of quality measures and how they are created, why quality measures matter when caring for adults with complex care needs in integrated systems, and how stakeholders can influence the quality measure development process.
Date Updated: 08/25/2016Introduction
The focus of the health care delivery system in the United States is shifting. It is no longer about the volume of services delivered, but rather the value of care provided. Demonstration models
have been deployed to determine how best to improve the quality of care for individuals with complex medical and social needs. These demonstrations and other initiatives strive to achieve
quality by coordinating health care, behavioral health care, and long-term services and supports (LTSS) including home and community-based services (HCBS). In order to determine if health care “value” has been obtained, clear and definable measures are necessary to assess care quality from the perspectives of people needing care, their loved ones, the provider community, and
payers. Making value-based care a reality – particularly for delivery systems that support older adults with chronic health conditions and daily living challenges – requires quality measures that
are responsive to the multi-faceted needs of these individuals while accurately evaluating the complexity of providing medical and non-medical services.
This policy brief provides an overview of the various types of quality measures, how they are created, why quality measures matter when caring for adults with complex care needs in integrated systems, and what stakeholders can do to influence the quality measure development process.
What are quality measures?
Health care quality measurement is defined as the process of using data to evaluate the performance of health plans and health care providers against recognized quality standards.2 High-quality health care is achieved when a person receives the right services at the right time, and in the right way to achieve the best possible health and quality of life.3
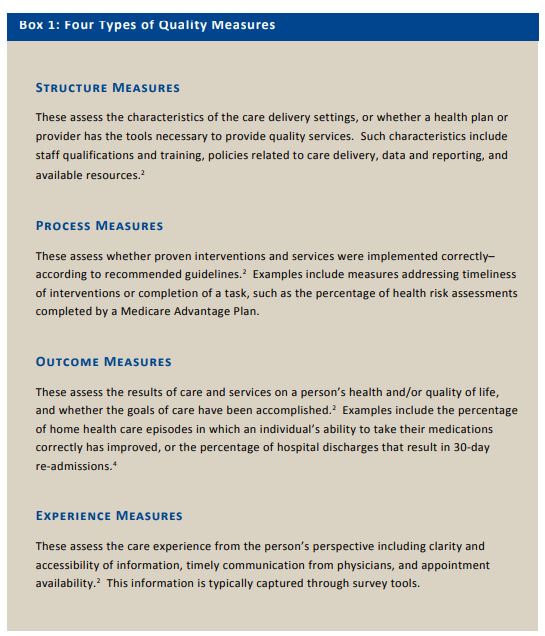
Quality measures are categorized into four types: structure, process, outcome, and experience (Box 1). Some measures look at specific steps like if and how services are provided, while others focus on results.5 Each type provides information about an aspect of quality, and when combined with the others, provides comprehensive insight on the experience of quality care.
How are quality measures made?
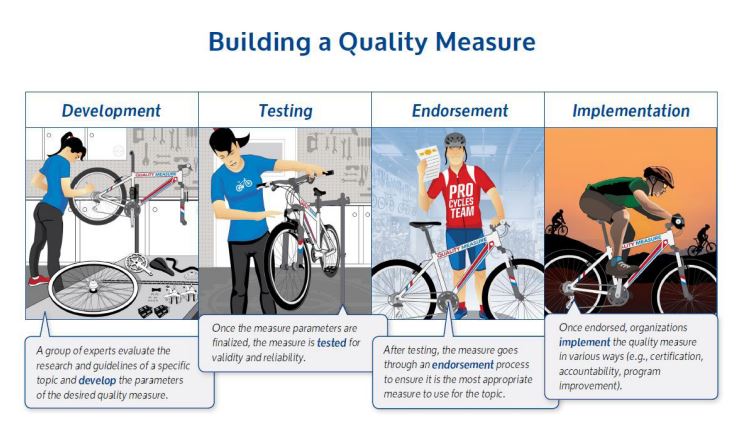
Building effective quality measures begins with the establishment of a framework with clear priorities to guide the quality development process. Quality measures are borne from evidencebased research, which in turn spurs clinical guidelines and standards that set goals for what should happen in health care delivery.2 After setting clear priorities, the process to create a quality
measure passes through four stages: development, testing, endorsement, and implementation.
Development: This typically involves convening a group of experts to evaluate the research and guidelines, and define the parameters of a quality measure. Such parameters include the relevancy of the measure, what the measure will evaluate, the feasibility of the measure, and how the data will be collected.2 Measure developers usually include national associations, universities, public agencies such as the Centers for Medicare & Medicaid Services (CMS), medical groups, health plans, and nonprofit organizations such as the National Committee for Quality Assurance (NCQA).6
Testing: Once the parameters of a measure are determined, the measure must be tested to ensure its validity (does it measure what is intended?) and reliability (can the finding be replicated across similar conditions?). The same organizations that develop measures often test them.2 The process of developing and testing measures takes significant time, e.g., a year. To support more efficient development and testing of measures, the National Quality Forum (NQF) established the Measure Incubator, which connects groups interested in specific measure concepts with measure development experts, financial and technical resources, and data.7
Endorsement: After a measure has been tested, it may be submitted for endorsement by professional societies and/or consumer groups who evaluate the appropriateness of the measure by considering its validity, reliability, usability, relevance, and feasibility. The endorsement process also allows stakeholders to evaluate and provide feedback on proposed measures. NQF is one such organization that endorses measures.8
Implementation: Endorsed quality measures are typically implemented by government agencies such as CMS and states, as well as health plans and providers.2 Entities across the delivery system use endorsed measures for a variety of external and internal purposes (discussed on page 6). Quality measures need ongoing monitoring and updating to ensure continued alignment with evolving best practices.
Why do quality measures matter for systems?
Endorsed and implemented quality measures have a variety of purposes throughout health care and can be used to foster change in delivery systems in external and internal ways.
External: Quality measures can be used as a basis for reimbursement. Payers, including CMS, use quality rankings as a basis for reimbursement, particularly in new and emerging valuebased purchasing arrangements. Regulators use quality measures for accountability to ensure health and quality of care meets established standards. They are also used in the accreditation and certification of providers. Finally, quality measures can be used by health care consumers as a tool for identifying and selecting providers.
Quality Measures Drive:
• Improved outcomes
• Informed care choices
• Payment based on performance
Internal: Health care plans and providers use quality measures to ensure appropriate care is provided and to identify opportunities for system improvement. Data for such quality measures can come from claims and patient surveys. These entities can also use this information to communicate positive results in order to support business development and marketing
activities.
Why do quality measures matter for adults with complex care needs?
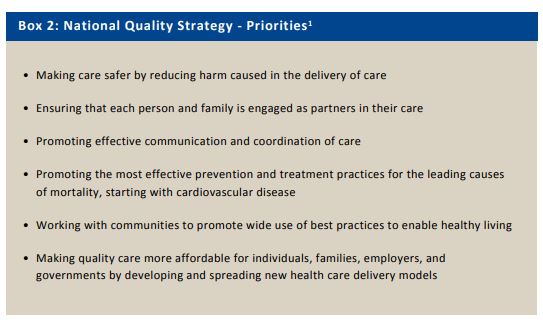
Emphasizing the importance of quality, in 2011, the Department of Health and Human Services (HHS) published the National Strategy for Quality Improvement in Health Care (National Quality Strategy; Box 2). This strategy included three broad goals to provide better care, improve health, and reduce cost, often referred to as the “Triple Aim.” HHS and CMS use the Triple Aim and supporting priorities to assess and guide advancement in quality programs, initiatives, and regulations.1
These priorities have influenced the development of the financial alignment demonstration for individuals eligible for both Medicare and Medicaid, and other initiatives working to coordinate health care, behavioral health care, and LTSS for individuals with health and daily living needs. Yet, due to limited standardized quality measures, HHS has not been able to fully assess core elements of integrated systems of care including: access to LTSS, coordination between medical care and LTSS, and the extent to which care planning and delivery is based on needs and preferences of the individual receiving care. Instead, measures have generally focused on improving single medicalconditions or processes (e.g., getting a flu shot) or structures and processes inside one aspect of the care delivery system (e.g., transitions from the emergency department to an inpatient hospital bed). Recognizing the profound influence that quality measures have on systems of care, it is critical that standardized measures are being developed that focus on improving medical and LTSS services for adults with complex care needs in integrated systems.
There has historically been little guidance as to what a quality system for adults with complex care needs would look like. However, much work is underway to create new quality measures. In 2016, HHS and CMS issued the Medicaid and CHIP Managed Care Final Rule with directives to states to strengthen the delivery of LTSS, including incorporating LTSS-specific elements into quality strategies.9 NCQA is also piloting standards for community-based organizations and health plans to assess coordination of LTSS.10
A recent paper, What Matters Most: Essential Attributes of a High-Quality System of Care for Adults with Complex Care Needs, reflects consensus from a national working group that provided guidance for system transformation and evaluation efforts.11 It highlights the need for quality measures that address a person-centered perspective in addition to current clinically-oriented and system-based measures. Adults with complex care needs value a high-quality system of care where individuals are able to live their lives with services and supports reflecting their values and preferences in the least restrictive, most independent setting possible with access to a delivery system that respects and supports their choices and decisions.
How stakeholders can influence quality measure development and selection?
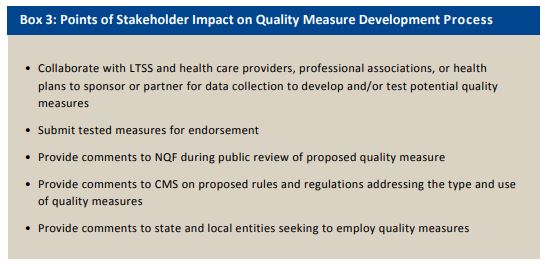
Stakeholders can contribute to identifying and creating quality measures during any one of the four stages described above. Box 3 outlines potential points of stakeholder impact on the quality
measure development process. Government agencies and nonprofit organizations (e.g., NQF) that endorse measures routinely provide opportunity for public comment on endorsement,
recommended uses, and gaps in quality measurement. A new federal law now allows CMS to consider measures beyond those that have been formally endorsed by allowing submission of
quality measures from content in peer reviewed journals or that meet other specific criteria.12,13 These comment opportunities allow stakeholders to not only weigh in on proposed measures but
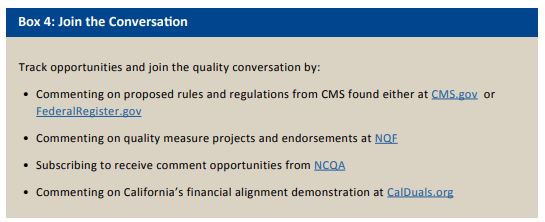
also recommend measures and data sets that can help shape quality measurement. Box 4 provides some examples of how stakeholders can join the quality measurement conversation and participate in shaping the next generation of systems for adults with complex care needs.
National quality measures have broad and deep impact in shaping systems of care. As the health care and LTSS delivery systems evolve, establishing quality measures to address identified gaps
and stakeholder comments to CMS can help inform how quality is assessed. It is challenging to measure quality, especially in systems of care for adults with complex care needs that include
health care and LTSS. With the expertise of stakeholders across the health care and LTSS delivery system, quality measures can be created that evaluate care delivery and person-centered
experiences.
Download the publication for all links, visuals and complete references.
Continue Reading
This policy brief provides an introduction to The SCAN Foundation’s CLASS Technical Assistance Brief Series, which explores many of the critical issues to be considered for successfully implementing CLASS.
This policy brief describes the broad needs of individuals with disability and the wide range of supportive and environmental solutions that can allow for the most independent living possible. It suggests how findings on social and environmental supports for individuals with disability can inform implementation of CLASS.
This policy brief provides background on the historical development of benefit eligibility triggers in the private long-term care insurance market. Understanding how these triggers came into being can provide important information to those charged with implementing the CLASS Plan.