Summary of the California Enacted 2021-22 Budget and Home- and Community-Based Services Spending Plan: Impact on Older Adults, People with Disabilities, and Their Caregivers
summary
Enacted on July 12, 2021, California’s 2021-22 budget addresses longstanding system challenges related to health care, long-term services and supports, workforce, and housing for older adults, people with disabilities, and their caregivers. It reflects the recommendations of the governor’s Master Plan for Aging issued earlier in 2021, and includes $4.6 billion to enhance access to home- and community-based services (HCBS), as outlined in California’s proposed HCBS Spending Plan.
Date Updated: 09/07/2021Overview
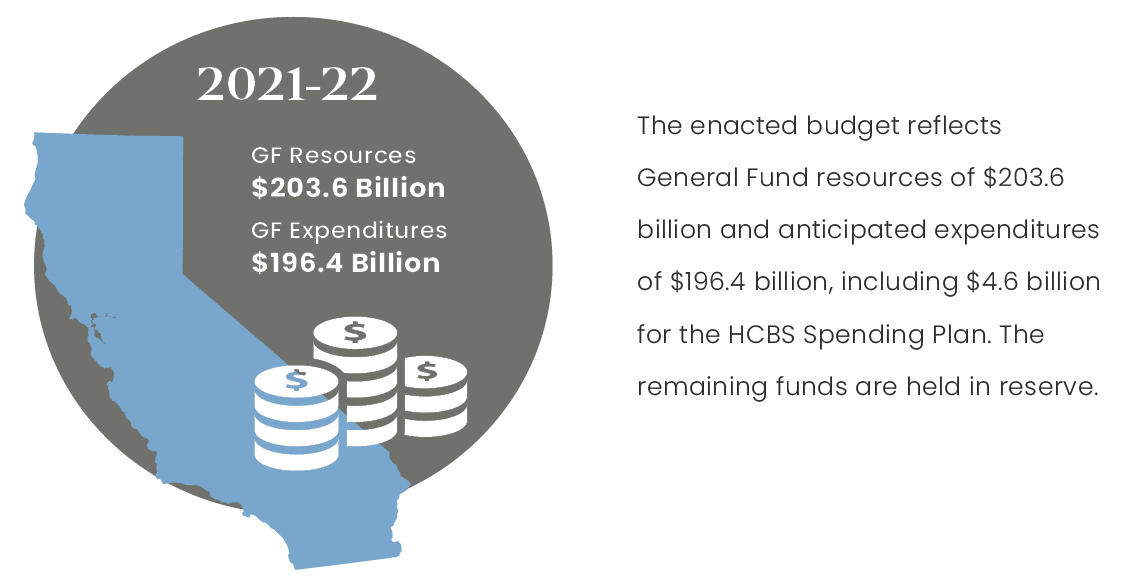
The 2021-22 budget includes significant investments to assist low- and middle-income Californians, strengthen the state’s infrastructure, and implement the Master Plan for Aging, among other priorities.1 As outlined below, the budget also includes spending authority for the state’s proposed $4.6 billion Home- and Community-Based Services Spending Plan, in accordance with the federal American Rescue Plan Act of 2021 (ARPA).2 Overall, the budget reflects total General Fund (GF) resources of $203.6 billion and anticipated expenditures of $196.4 billion, with the remainder held in reserves.1
A New Era for Aging in California
This past year, California’s low-income older adults, people with disabilities and caregivers, as well as Black, Latinx, Indigenous, Asian and Pacific Islander, and LGBTQ populations have experienced tremendous hardships. Today’s challenges magnify underlying system issues that for years have impacted the aging population, including workforce shortages, lack of access to housing and services, and fragmented health care and long-term services and supports (LTSS) systems.
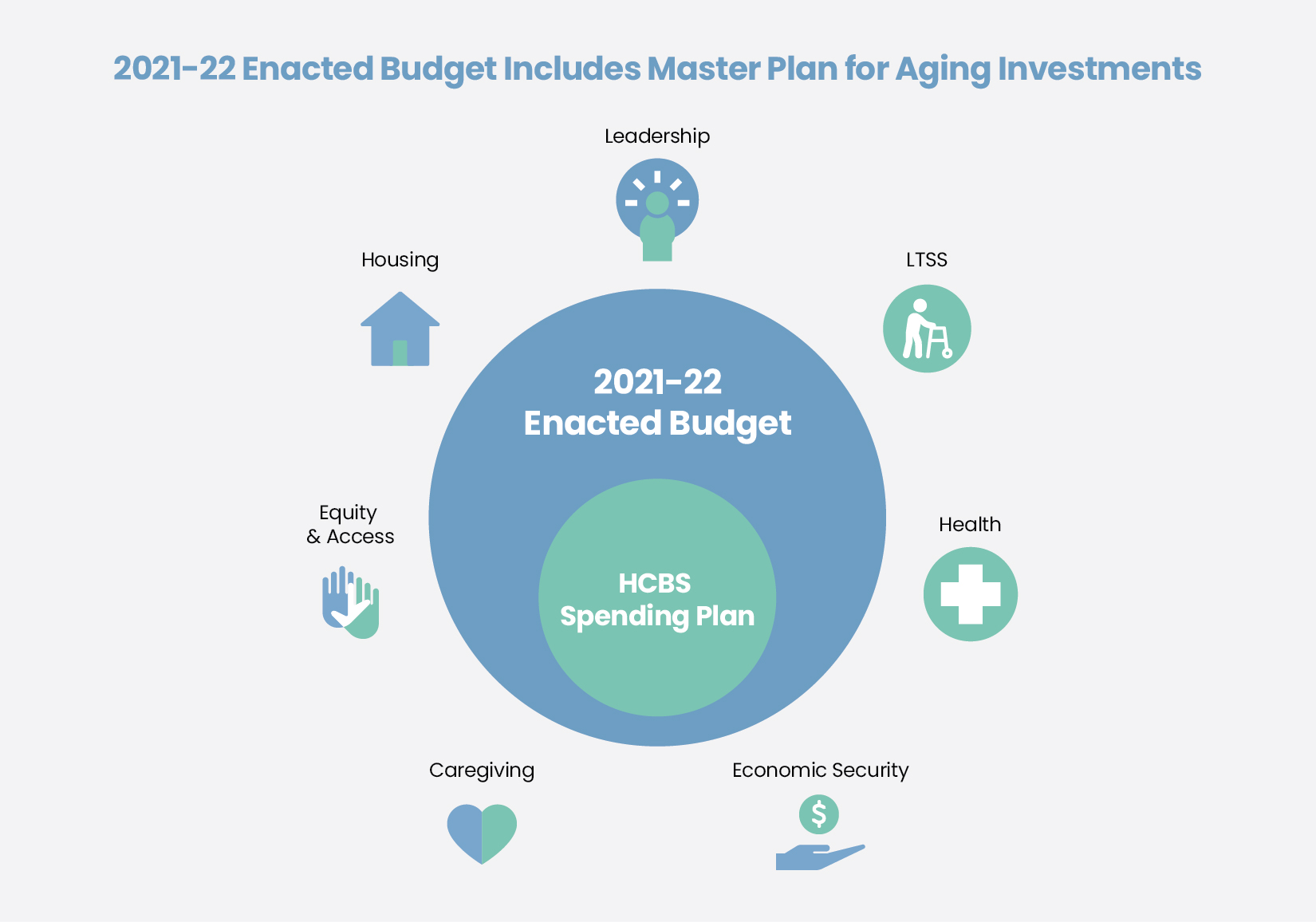
However, in this past year the state has shown that bold leadership, coupled with public/private partnership, can change this narrative. Grounded in principles of equity and inclusion, the Master Plan for Aging (Master Plan) is paving the way for broad-based system change across health care, LTSS, housing, and the workforce. The 2021-22 budget reflects unprecedented investments in the Master Plan. While there is still much work to do, the budget offers a very solid start to its 10-year implementation.
California’s 2021-22 Budget: Impact on Older Adults, People with Disabilities, and Family Caregivers
The enacted 2021-22 budget includes a range of new investments in line with the Master Plan, as outlined below. Several of these investments are supported through one-time funds and continued COVID-19 stimulus funding, all of which advance Master Plan implementation.1
| Table 1: State Leadership1,3 | ||
| Item | Action | 2021-22 Enacted Budget |
| Senior Advisor on Aging, Disability, and Alzheimer’s | Commitment to establish a position within the governor’s office to lead on cross-cabinet initiatives and cross-sector partnerships | $258,000 GF |
| Office of Medicare Innovation and Integration | Establishes a new office inside the Department of Health Care Services (DHCS) to focus on policy opportunities related to Medicare-only and dual-eligible populations | $602,000 ($452,000 GF) |
| Master Plan Leadership/ Operations | Funds 20 permanent positions within the California Department of Aging (CDA) for implementation of the Master Plan | $3.3 million GF |
| Health information Exchange | Calls on the California Health and Human Services Agency (CHHS) to lead information exchange efforts for health and social services | $2.5 million GF* |
The enacted budget includes significant health care investments that expand access to Medi-Cal and telehealth, and implement California Advancing and Innovating Medi-Cal (CalAIM) and other provisions highlighted in Table 2 below.
| Table 2: Health Care Affordability and Access1,4 | ||
| Item | Action | 2021-22 Enacted Budget |
| Medi-Cal Asset Test | Increases Medi-Cal asset limit to $130,000 for an individual (plus $65,000 for each additional household member) by July 1, 2022, and fully eliminates the asset limit by January 1, 2024 | $394 million ($197 million GF) in 2022-23 |
| Medi-Cal Expansion | Expands Medi-Cal to approximately 27,000 undocumented adults age 50 and older by May 1, 2022 | $67.3 million ($48 million GF)
$1.5 billion |
| Medi-Cal Optional Benefits | Repeals the suspension of Medi-Cal optional benefits including audiology and speech therapy services, incontinence creams and washes, optician/optical lab services, and podiatric services | $47 million ($15.6 million GF) |
| CalAIM | Implements CalAIM beginning January 1, 2022. The investment includes Enhanced Care Management (ECM), In Lieu of Services (ILOS) and other program elements | $1.6 billion
($650.7 million GF) |
| Telehealth | Expands and makes permanent certain telehealth COVID-19 flexibilities, and adds remote patient monitoring services as a Medi-Cal covered benefit | $151.1 million ($53.3 million GF) |
| Population Health Management Service | Creates a centralized data system of administrative and clinical data from DHCS, health plans, and providers | $315 million
($31.5 million GF)* |
| Alameda Wellness Respite Center | Provides funding for the Alameda Wellness Respite Center with services that include recuperative care, senior housing with medical services, and a homelessness resource center | $15 million GF* |
| Medically Tailored Meals | Funds medically tailored meals until it is available as an option for ILOS under CalAIM | $9.3 million GF* |
| Geriatric Medicine Workforce | Grows and diversifies the geriatric medicine workforce. Includes resources for Alzheimer’s disease training | $8 million GF* |
| Physician Orders for Life Sustaining Treatment (POLST) Registry | Establishes the electronic POLST Registry to ensure an individual’s treatment preferences are available during a medical emergency | $10 million GF
$750,000 GF |
The enacted budget includes investments to enhance LTSS system capacity, as reflected by the items outlined in Table 3 below.
| Table 3: Long-Term Services and Supports1 | ||
| Item | Action | 2021-22 Enacted Budget |
| In-Home Supportive Services (IHSS) | Makes permanent the IHSS back-up provider system to avoid caregiving disruptions due to emergencies | $12.8 million GF* |
| IHSS State/County Funding Ratio | Maintains the state/county ratio for non-federal costs of 65/35 amid increases in minimum wage | $57.3 million GF |
| IHSS – Elimination of 7 Percent Reduction | Eliminates the across-the-board 7 percent reduction in IHSS service hours | $248 million GF (2021-22)
$496 million GF (ongoing) |
| Office of Long-Term Care Patient Representative | Provides a public patient representative to nursing facility residents who are not able to make decisions for themselves and do not have a family representative | $2.5 million GF |
| Caregiver Resource Centers | Increases baseline funding for Caregiver Resource Centers | $10 million GF |
| Multipurpose Senior Services Program (MSSP) | Makes the MSSP rate increase permanent and increases MSSP slots to 2,497 | $6.3 million GF |
| Community-Based Adult Services (CBAS) | Provides 10 permanent positions in CDA for CBAS certification | $1.9 million ($800,000 GF) |
The enacted budget includes investments to support consumers in accessing the information and support needed to navigate the health care and LTSS systems, as outlined in the Table 4.
| Table 4: Consumer Information and Support1,5 | ||
| Item | Action | 2021-22 Enacted Budget |
| Aging and Disability Resource Connections (ADRC) | Funds 13 permanent positions for state operations to support the ADRC program | $2 million GF |
| Adult Protective Services | Expands Adult Protective Services to serve people age 60 and older | $70 million GF |
| Health Insurance Counseling and Advocacy Program (HICAP) |
Modernizes HICAP | Fund through 2022-23 |
| Local Assistance | Expands the ADRC program statewide and develops a statewide portal | $7.5 million GF (2021-22) |
| Medi-Cal Navigators for Medi-Medi Seniors | Provides navigators for people with Medicare and Medi-Cal | $12 million GF |
Additionally, the budget includes $24.5 million GF for a comprehensive package of services to address Alzheimer’s disease, as reflected in Table 5.1 Funding for the Alzheimer’s disease workforce development is included as part of the workforce development funding in Table 2. Additionally, funding for Alzheimer’s Day Care and Resource Centers is outlined in the Home- and Community- Based Services (HCBS) Spending Plan in Table 9.
| Table 5: Alzheimer’s Disease Prevention and Preparedness1,5-7 | ||
| Item | Action | 2021-22 Enacted Budget |
| Alzheimer’s Disease Standards of Care | Expands standards of care to address Alzheimer’s disease | $4.5 million GF* |
| Alzheimer’s Disease Research | Addresses disparities and promotes equity in Alzheimer’s disease research | $4 million GF* |
| Alzheimer’s Disease Brain Health Campaign | Launches a public education campaign on brain health | $10 million GF* |
| Alzheimer’s Disease Caregiver Training | Provides caregiver training and certification in Alzheimer’s disease | $4 million GF* |
| Dementia-Friendly Communities | Provides grants to help communities become dementia-friendly | $2 million GF* |
The enacted budget enhances access to affordable housing and services for those experiencing homelessness, with new investments supported by a combination of federal and state dollars. Table 6 reflects the housing items that could directly impact older adults and people with disabilities.
| Table 6: Housing and Homelessness1 | ||
| Item | Action | 2021-22 Enacted Budget |
| Accessory Dwelling Units | Expands available funding for Accessory Dwelling Units | $81 million* |
| Preservation of Affordable Housing | Allows the state to preserve existing affordable housing units as affordability covenants expire | $300 million* |
| Housing and Disability Advocacy Program (HDAP) |
Offers outreach, case management, disability advocacy, and housing assistance through the HDAP to older adults and people with disabilities experiencing homelessness | $300 million GF (over 2 years) |
| HomeSafe | Provides health, safety, and housing supports for older and vulnerable adults involved in or at risk of involvement in Adult Protective Services | $185 million GF (over 2 years) |
| Supportive Services for Formerly Homeless Veterans | Supports aging veterans and veterans with disabilities who have experienced chronic homelessness | $25 million GF |
| Project Homekey | Provides Project Homekey grants to local public entities to convert underused properties to housing for the homeless | $2.75 billion* (over 2 years) |
| Project Roomkey | Transitions Project Roomkey program participants into permanent housing | $150 million GF |
The enacted budget invests in economic security and food access initiatives to assist California’s low-income older adults, people with disabilities, and others in obtaining income support and food assistance, as outlined in Table 7.
| Table 7: Economic Security and Food Access1,5 | ||
| Item | Description | 2021-22 Enacted Budget |
| State Supplementary Payment (SSP), Cash Assistance Program for Immigrants, and California Veterans Cash Benefit | Increases the SSP, Cash Assistance Program for Immigrants, and California Veterans Cash Benefit grants by rescinding a portion of the cost-of-living adjustment cuts made during the recession (remaining cuts intended to be rescinded in 2023-24) | $291.3 million GF |
| Senior Nutrition | Provides additional funding for increased meals, including home-delivered meals and congregate sites | $14.3 million GF |
| CalFresh Expansion – Older Adults Outreach | Assists older adults eligible for Supplemental Security Income (SSI) and SSP with applying for CalFresh benefits | $2 million
($1.1 million GF) |
| Food Banks | Supports Emergency Food Assistance Program providers, food banks, tribes, and tribal organizations to mitigate increased food needs related to COVID-19 | $110 million GF* |
| Food Banks | Supports food bank capacity enhancement and climate resilience | $182 million GF* |
| Supplemental Nutrition Benefit and Transitional Nutritional Benefit | Adjusts benefit amounts to mitigate the effects of the elimination of the SSI Cash-Out policy | $22.3 million GF |
| California Food Assistance Program Emergency Allotments | Allows households to receive maximum allowable allotment based on household size | $11.4 million GF* |
The enacted budget also focuses on equity, as well as efforts to inform responses for future emergencies and improve language access across the CHHS department and programs that serve older adults and people with disabilities, as reflected in Table 8.
| Table 8: Health Equity and Access1 | ||
| Item | Action | 2021-22 Enacted Budget |
| Health Care Service Plan Health Equity and Quality Reviews | Establishes health equity and quality standards and enforcement for all Department of Managed Health Care licensed health plans that are full-service or behavioral health plans |
$1.2 million ($148,000 GF) |
| Racial/Implicit Bias Training | Provides funds for racial/implicit bias training for county staff | $3 million GF |
| Pandemic Response Review | CHHS to conduct an analysis of the intersection of COVID-19, health disparities, and health equity to help inform any future response | $3 million GF* |
| Language Access Initiative | Establishes an initiative to improve and deliver language access services across CHHS programs | $20 million GF* |
| Medi-Cal Translation Materials | Allows ongoing field testing of translated Medi-Cal materials | $2 million ($1 million GF) |
California’s Proposed Home- and Community-Based Services Spending Plan
On March 11, 2021, President Biden signed the American Rescue Plan Act of 2021 (ARPA) to assist state and local governments with fiscal recovery from the COVID-19 pandemic. Among other provisions, ARPA includes a temporary 10 percent increase to states’ Federal Medical Assistance Percentage (FMAP) to provide additional support for Medicaid HCBS.2
The enhanced federal funding provides an opportunity to make meaningful investments in HCBS programs serving older adults, people with disabilities, and caregivers—as well as people with developmental disabilities, people with behavioral health needs, and those experiencing homelessness.
The 2021-22 Budget and the HCBS Spending Plan
On July 12, California submitted its proposed $4.6 billion Home and Community-Based Services Spending Plan (Spending Plan) to the federal government, which is currently under review by its Centers for Medicare & Medicaid Services (CMS). The Spending Plan is a combination of the $3 billion in enhanced federal match provided by ARPA through 2023-24, and $1.6 billion standard GF and FMAP for Medi- Cal covered services.8
The enacted budget establishes a Home- and Community-Based Services American Rescue Plan Fund (HCBS ARPA Fund), which will pay for Spending Plan items. The HCBS ARPA Fund includes the approximately $3 billion enhanced federal match provided by ARPA, allocated to the following:
- $1.5 billion to reduce and replace the General Fund cost of HCBS proposals included in the budget.
- $1.5 billion to fund HCBS augmentations identified by the Secretary of Health and Human Services Agency and the Department of Finance, in addition to proposals already included in the budget.9
California’s proposed Spending Plan includes investments seeking to build capacity and transform the system through workforce development, HCBS navigation, transition, enhanced HCBS capacity, and HCBS infrastructure and support. The following proposed investments include key areas that impact older adults, people with disabilities, and family caregivers. These are, again, in alignment with the Master Plan.8†
| Table 9: HCBS ARPA Spending Plan1,5,8-11 | |||
| Item | Action | Spending Plan Total Funds (TF) | Funding Included in the Budget‡ |
| Workforce | |||
| IHSS Career Pathways | Incentivizes and funds career paths for IHSS providers | $295.1 million TF* | √ |
| Direct Care Workforce (non-IHSS) Training and Stipends | Incentivizes, supports, and funds career paths for non-IHSS providers | $150 million TF* | |
| IHSS HCBS Care Economy Payments | Provides a one-time $500 payment to current IHSS providers who worked a minimum of two months between March 2020 and March 2021 | $274.6 million TF* | |
| Non-IHSS HCBS Care Economy Payments | Provides a one-time $500 payment to current direct care, non-IHSS providers of Medi-Cal HCBS who worked a minimum of two months between March 2020 and March 2021 | $12.5 million TF* | |
| Home- and Community-Based Clinical Workforce | Provides grants to expand training for home-based clinical care | $75 million TF* | |
| Providing Access and Transforming Health (PATH) | Provides funds to recruit and train homeless and direct care workforce, as well as support ECM and CalAIM ILOS provider capacity building and infrastructure investments | $100 million TF* |
√ |
| Traumatic Brain Injury (TBI) Program | Expands the capacity of existing TBI sites and stands up six new sites in underserved areas | $5 million TF* | |
| HCBS Navigation | |||
| Aging and Disability Resource Connections (ADRC) | Supports interoperability between the proposed ADRC technology and data systems with community-based organizations (CBOs), health plans, and counties in line with the CalAIM goals | $5 million TF* | |
| Dementia Aware and Geriatric/Dementia Continuing Education | Supports development of an annual cognitive health assessment, provider dementia care training/continuing education, and referral protocols | $25 million TF* | |
| Language Access and Cultural Competency Orientations and Translations | Supports identification of documents for translation, threshold languages, and coordination of interpretation and translation services for regional center consumers and families | 45.8 million TF* | √ |
| CalBridge Behavioral Health Pilot | Provides grants to acute care hospitals to support hiring trained behavioral health navigators in emergency departments to screen patients, and offer intervention and referrals to services | $40 million TF* | |
| HCBS Transitions | |||
| Community Based Residential Continuum Pilots | Supports managed care plans in providing access to home-based medical, behavioral health, and personal care services | $297.7 million TF* | |
| Assisted Living Waiver (ALW) | Adds 7,000 slots to the ALW in an effort to eliminate the current waitlist | $254.7 million TF
$38 million (ongoing) |
|
| Housing and Homelessness Incentive Program | Incentivizes Medi-Cal managed care plans to make investments and progress in addressing homelessness | $1.3 billion TF* | |
| Community Care Expansion Program | Acquires and rehabilitates Adult Residential Facilities and Residential Care Facilities of the Elderly to expand housing for homeless, low-income older adults, or those at risk of homelessness | $348.3 million TF* | √ |
| Services: Enhancing HCBS Capacity | |||
| Nursing Home Recovery and Innovation | Accelerates innovations for nursing home facilities that drive quality care (e.g., Small Home pilot) | $2 million TF* | |
| Alzheimer’s Day Care Resource Centers | Provides funding for Adult Day and Adult Day Health Centers to offer dementia-capable services | $5 million TF* | |
| Older Adult Resiliency and Recovery | Provides additional funding based on local need for programs including: Senior Nutrition, Senior Legal Aid, Home Modifications and Fall Prevention, Behavioral Health Line, Senior Digital Connections, Family Caregiver Support, Senior Employment Opportunities, Elder Abuse Prevention, and Aging and Disability Resource Connections | $106 million TF* (over 3 years) |
√ |
| Adult Family Homes | Provides funding for an Adult Family Homes pilot in one county. Through this model, up to two older adults reside with a family unit | $9 million TF
$2.6 million |
|
| HCBS Infrastructure and Support | |||
| LTSS Data Transparency | Seeks to improve LTSS data transparency by developing an LTSS data dashboard linked with utilization, quality, cost, and demographic data across LTSS programs | $2 million TF* | |
| Access to Technology | Provides grants to county human services agencies to increase access to technology for older adults and adults with disabilities | $50 million TF* | √ |
| Senior Nutrition Infrastructure | Provides funding for capacity and infrastructure improvements for senior nutrition programs | $40 million TF* | √ |
A Closing Note on Advancing the Master Plan for Aging: Four Recommendations for Gubernatorial and Legislative Leadership and Stakeholder Engagement
The historic investments included in the 2021-22 budget and the proposed HCBS Spending Plan offer great potential to advance system transformation with a focus on equity. The Master Plan provides a structure to prioritize and guide use of these funds to be the most impactful and equitable. However, this will require strong and sustained state and legislative leadership as well as stakeholder engagement.
The following recommendations speak to the important role the California Legislature, the governor, and stakeholders play in advancing Master Plan implementation with a focus on equity in the years ahead.
- Senior Advisor for Aging, Disability and Alzheimer’s: At the gubernatorial level, there is need for coordinated, engaged leadership addressing aging issues across multiple state agencies. The enacted budget includes resources for a Senior Advisor for Aging, Disability and Alzheimer’s. While this is a very small piece of the state’s $204 billion budget, it holds the potential to create long-term change for California’s older adults, people with disabilities, and family caregivers. Filling this position in the near future is imperative as it will play a key role in advancing Master Plan efforts.
- Legislative Oversight and Leadership: The Legislature plays an important role in overseeing key policy initiatives of the Master Plan, and ensuring the state is held accountable for implementation. To this end, legislative oversight hearings on both the Master Plan and the HCBS Spending Plan are critical to identifying issues and ensuring successful implementation. Additionally, to build legislative leadership, the Legislature could establish an Aging and Disability Caucus with legislators committed to advancing system transformation.
- Stakeholder Engagement and Coordinated Advocacy: To ensure an equitable approach to Master Plan implementation, it is important that the state hear from diverse voices representing older adults, people with disabilities, and family caregivers. Stakeholders could benefit from developing a coordinated voice through which to advocate for Master Plan priorities. Additionally, with multiple stakeholder groups serving across departments§, there is potential for overlapping/duplicative discussions and confusion about areas of responsibility. The Disability and Aging Community Living Advisory Committee (DACLAC) focuses on the tenets of community living, and includes representation across aging, disability, developmental disability, and behavioral health populations. As such, DACLAC is primed to serve as the leading stakeholder group providing input to help guide the state and Legislature with HCBS Spending Plan implementation.
- Local Planning: Implementation of the Master Plan relies on strong local engagement and The California Advocacy Network is a statewide collaboration involving nearly 1,000 organizations including CBOs, aging and disability service and advocacy groups, and consumer and provider organizations. These local partners play a critical role in working with public and private partners to address local needs. These efforts should be leveraged to build out local-level plans, particularly in under-resourced and underserved communities, using the Master Plan’s Local Playbook as a template.
Download the publication for all visuals and complete references.
Continue Reading
This policy brief provides an introduction to The SCAN Foundation’s CLASS Technical Assistance Brief Series, which explores many of the critical issues to be considered for successfully implementing CLASS.
This policy brief describes the broad needs of individuals with disability and the wide range of supportive and environmental solutions that can allow for the most independent living possible. It suggests how findings on social and environmental supports for individuals with disability can inform implementation of CLASS.
This policy brief provides background on the historical development of benefit eligibility triggers in the private long-term care insurance market. Understanding how these triggers came into being can provide important information to those charged with implementing the CLASS Plan.